Insomnia and Brain Health: The Neurofeedback Connection
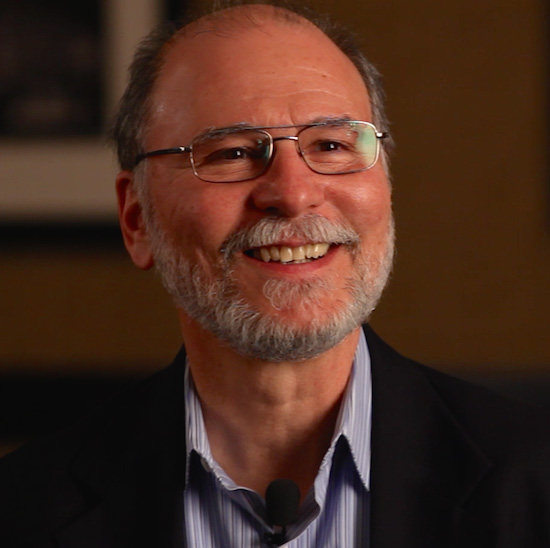 It only seems appropriate to close out Insomnia Awareness Month by interviewing neuroscientist and certified sleep medicine specialist, Dr. Edward O’Malley of Fairfield, Connecticut. He has utilized NeurOptimal® Neurofeedback as a cornerstone of his practice for many years now. Basically, Dr. O’Malley is so good at his job that he puts people to sleep; and that’s a good thing. The vast majority of clients who darken his doors are staring at the ceiling most of the night.
It only seems appropriate to close out Insomnia Awareness Month by interviewing neuroscientist and certified sleep medicine specialist, Dr. Edward O’Malley of Fairfield, Connecticut. He has utilized NeurOptimal® Neurofeedback as a cornerstone of his practice for many years now. Basically, Dr. O’Malley is so good at his job that he puts people to sleep; and that’s a good thing. The vast majority of clients who darken his doors are staring at the ceiling most of the night.
Insomnia is a growing public health problem. According to the National Sleep Foundation, 48% of Americans suffer from occasional insomnia, while a 22% report nightly sleep interruptions. Recent studies show extended sleep deprivation can have serious consequences for one’s health; most especially one’s brain health. Dr. O’Malley explains: Phamaceuticals offer a temporary ‘cure’ but the risk addiction with certain drugs can be very high. That’s why O’Malley has turned to using neurofeedback as it has proven to be one of the best natural remedies for insomnia available.
1. What is the connection between quality sleep and brain health?
There is a bidirectional relationship between good sleep and brain health. While the need for good sleep may be obvious, the other direction may not be. An ailing brain, for extreme examples, like Alzheimer’s or Parkinson’s diseases, results in severely fragmented sleep. This severely disturbed sleep then interferes with normal brain processing which then worsens the brain disorder. A less extreme but common example, and unfortunately equally disturbing, is chronic stress, including chronic sleep restriction (you know, the “burning the candle at both ends” syndrome), both of which create a worsening sleep condition which then further exacerbates the stress.
2. What happens to our brains during sleep?
Our brains need to clear out the daily waste products generated by waking cognition. The only physiological state in which this happens is sleep. So, no or reduced sleep allows for the accumulation of these toxic (to brain cells) waste products which then lead to brain cell death. This also provides a mechanism for the vicious cycle, because less sleep, increased waste, brain cell death leads to worse sleep, more toxic byproduct buildup, more cell death etc.
3. What does research say about connection between sleep and “emotional” disorders like anxiety or depression?
Again, these are “chicken or egg” phenomena in terms of the direction of causation. We know that insomnia is an independent risk factor for mood disorders (depression, anxiety bipolar etc) and mood disorders are an independent risk factor for developing insomnia. Indeed, often the initial complaint of both types of disorders is disturbed sleep. It is unclear whether the brain changes associated with either cause the other. But it follows that improved brain function can improve both classes of disorders.
4. What are some of the more interesting recent developments you’ve seen in the science of sleep?
The recent finding that the sleep state is required for brain health and lack of adequate sleep potentially underlies neurodegenerative disorders like Alzheimer’s and other dementias, and may contribute to general aging itself.
5. What have you observed about NeurOptimal® neurofeedback and sleep improvement?
NeurOptimal® seems to improve sleep across the full spectrum of medical disorders! It makes sense that improved brain function (resilience and flexibility) would result in improved sleep (and vice versa), as noted above. I always recommend at least one night of sleep between NeurOptimal® neurofeedback sessions to allow the brain to integrate this new information.
6. What’s the most important thing you’ve learned in your experience with people suffering with insomnia?
That people’s daily waking life activity is at least as important as what they do to obtain a good night’s sleep.
7. What’s the most surprising/unexpected thing you’ve learned about sleep disorders?
Same as above essentially–that general well-being, i.e., a life well-lived, is at least as important as the physiology of sleep.
